Patients with CCCA May be at Risk for Type 2 Diabetes.
Two prior studies by Coogan et al and Kyei et al suggested that women with Central centrifugal cicatricial alopecia (CCCA) are at risk for diabetes. A third study now supports this notion.
The study was a study of black women between the ages of 18 and 74 who presented over a 4 year period to the Hospital of the University of Pennsylvania. Electronic databases were searched to find patients with a clinical diagnosis of CCCAA and also those with a biopsy-proven diagnosis too.
Using the “hemoglobin A1c” blood test as a marker for diabetes, the researchers showed that 58 % of 181 women with CCCA had an elevated hemoglobin A1c test result that suggested a diagnosis of diabetes. In contrast, 43 % of 16, 454 women who did not have CCCA had an elevated hemoglobin A1c test result that suggested a diagnosis of diabetes.
The researchers also looked at the data another way. Of women in the study with a clinical diagnosis CCCA, 37 % had a history of diabetes compared to just 12 % of control patients. All in all, these data suggested that women with CCCA are at a 4.13 fold increased risk for diabetes compared to race, age and sex matched controls.
Of women in the study with a biopsy-proven diagnosis of CCCA, 32 % had a history of diabetes compared to just 12 % of control patients. All in all, this data suggested that women with CCCA are at a 3.26 fold increased risk for diabetes.
Conclusion and Summary
Women wth CCCA, including non-obese women, are at increased risk for diabetes. Appropriate diabetes screening is needed for all patients with CCCA.
Reference
Roche et al. Association of type 2 diabetes with central centrifugal cicatricial alopecia: A follow-up study. J Am Acad Dermatol. 2021 Feb 18;S0190-9622(21)00361-3
Coogan PF et al. Association of type 2 iabetes with central-scalp hair loss in a large cohort study of African American women. .Int J Womens Dermatol. 2019 Jun 6;5(4):261-266.
Kyei et al. Medical and environmental risk factors for the development of central centrifugal cicatricial alopecia: a population study..Arch Dermatol. 2011 Aug;147(8):909-14.
Women with CCCA May be At a 3 Fold Increased Risk for Breast Cancer.
Central centrifugal cicatricial alopecia (CCCA) is a scarring alopecia that affects black women age 35-60. A new study from the University of Pennsylvania leads us in a potentially new direction in understandng comorbidies associated with CCCA.
The researchers performed a cross-sectional study of black women aged 18 years or older who presented to the University of Pennsylvania Health System over the 4 year period April 13, 2016, to April 13, 2020. Patients with CCCA were identified in electronic databases based on coding. Patients with breast cancer or colon cancer were also identified by standard coding.
There were over, 225,000 black women treated during this four year period within the University of PennsylvaniaHealth System. There were 742 patients identified with a clinical diagnosis of CCCA. 4.7 % of these women had a diagnosis of breast cancer compared to 1.8 % of controls. This corresponded to an odds ratio of 2.61. 149 of the 742 patients had a biopsy that confirmed the diagnosis of CCCA. 4.4 % of these 149 patients had a diagnosis of breast cancer corresponding again to an evaluated odds ratio of 2.49.
There was no increased risk of colon cancer among women with CCCA.
Summary and Comment
This is an important study and opens the door for other confirmatory studies. Theses data suggest that women with CCCA may be an increased risk for breast cancer.
Reference
Brown-Korsah JB et al. Association of breast and colorectal cancer in patients with central centrifugal cicatricial alopecia: A retrospective, cross-sectional pilot study. Journal of the American Academy of Dermatology 2021 Mar;84(3):859-860.
Is there a decreased risk of skin cancer in patients with AA?
Alopecia areata is an autoimmune condition. Recent studies have suggested that a closely related autoimmune condition called vitiligo (whereby skin cells lose pigment) may be associated with a decreased risk of skin cancer.
A number of studies to date have suggested that patients with alopecia areata may be at decreased risk for skin cancer.
Miller R et al. 2015
In a 2015 study, researchers evaluated 584 patients with alopecia areata and compared data to 172 controls. Data showed that patients with alopepcia areata had a reduced risk of squamous cell carincoma (0.51 % vs 0.58% with p=0.012). There was a trend for a reduced risk of basal cell carcinoma (1.54% vs. 3.48% (P=0.10), and malignant melanoma (0.51% vs. 1.74% (P=0.10).
Mostaghimi et al 2016
In a 2016 study, researchers from Harvard looked at the the risk of skin cancer in patents with alopecia areata compared to patients who did not have alopecia areata. A incidence of skin cancer in 1414 patients with alopecia areata was compared to the risk of skin cancer in 4242 patients who did not have alopecia areata.
Overall, there were fewer patients with alopecia areata who were diagnosed with basal cell and squamous cell skin cancers compared to patients who did not have alopecia areata. Interestingly, there was a slightly decreased risk of melanoma as well.
CONCLUSION
Patients with alopecia areata appear to have a reduction in the risk of squamous cell and possibly other skin cancers as well.
REFERENCE:
Mostaghimi et al. Reduced incidence of skin cancer in patients with alopecia areata: A retrospective cohort study. Cancer Epidemiology 2016
Miller R et al. Prevalence of Comorbid Conditions and Sun-Induced Skin Cancers in Patients with Alopecia Areata. J Investig Dermatol Symp Proc . 2015 Nov;17(2):61-2. doi: 10.1038/jidsymp.2015.44.
The Bidirectional Relationship between IBS and Alopecia Areata
Alopecia areata (AA) and irritable bowel syndrome (IBS) are two distinct diseases that share a similar pathophysiology; however, the relationship between these two diseases is not fully understood.
In 2017, Conic and colleagues set out to retrospectively review the clinical features of patients with alopecia areata that were seen at the Cleveland Clinic from 2005 to 2014. In total, data from 504 patients was tabulated, and as a comparison group, 172 patients with seborrheic dermatitis were also reviewed. The key bowel diseases that were studied were celiac disease, inflammatory bowel disease and irritable bowel syndrome. Interestingly, the incidence of irritable bowel syndrome was increased in patients with AA but there was no increase in inflammatory bowel disease and no increase in celiac disease.
Ying-Xiu Dai et al. 2022
In 2022, the authors set out to investigate the bidirectional relationship between AA and IBS. Participants were recruited from the National Health Insurance Research Database in Taiwan. The study participants included 5446 patients with AA and 21 784 matched controls to assess the risk of IBS, and 56 429 patients with IBS and 225 716 matched controls to assess the risk of AA.
What were the results?
After adjustment for potential confounders, patients with AA had an aHR of 5.20 [95% confidence interval (CI) 3.97-6.82] for IBS in comparison with the controls. Furthermore, compared with the controls, IBS patients had an aHR of 5.38 (95% CI 3.95-7.34) for AA.
Conclusion:
This study supports the notion that AA is bidirectionally associated with IBS. Further investigation is needed to elucidate the shared pathogenesis underlying these two diseases.
REFERENCE
Ying-Xiu Dai et al. Bidirectional association between alopecia areata and irritable bowel syndrome: A nationwide population-based cohort study. Australas J Dermatol . 2022 May;63(2):e127-e132. doi: 10.1111/ajd.13809. Epub 2022 Feb 23.
Conic R et al. Comorbidities in patients with alopecia areata. J Am Acad Dermatol . 2017 Apr;76(4):755-757. doi: 10.1016/j.jaad.2016.12.007.
Meta-Analysis Highlights Association Between Alopecia Areata and Hearing Loss.
Several studies in the past have suggested an association between alopecia areata and hearing loss.
Briefly, alopecia areata is an autoimmune disease and follicular melanocytes are thought to be one of the important targets of the activated immune system. Melanocytes have a key role in the auditory system, so it’s not surprising that researchers have examined the link between alopecia areata and hearing loss.
Sensorineural hearing loss (SNHL) is the most common type and accounts for the majority of all hearing loss in the general population. SNHL refers to any cause of hearing loss due to a pathology of the cochlea, auditory nerve, or central nervous system. In other words, sensorineural hearing loss results from damage to the hair cells within the inner ear, the vestibulocochlear nerve, or the brain's central processing centers
Lien KH et al. 2023
In a new study, authors performed a systematic review using five case-control studies and one cohort study. The meta-analysis showed AA patients had significantly higher mean differences in pure tone hearing thresholds at 4000 Hz and 12000 to 12500 Hz. The meta-analysis also found a three fold increased odds for SNHL among patients with AA (OR 3.18; 95% CI 2.06-4.89).
The hearing loss was most marked at 12000 to 12500 Hz. However, among 250 to 8000 Hz, the range which most sounds of daily conversations occur, only 4000 Hz showed significant difference in the author’s meta-analysis.
All in all, the authors here concluded that alopecia areata is associated with an increase of SNHL, especially at high frequencies. The authors remind us that high frequency hearing loss is often neglected by patients but may present with tinnitus. The authors proposed that consultation with an audiologist may be indicated if patients with alopecia areata present with hearing abnormalities such as hearing loss or tinnitus.
High frequency hearing loss is a common type of hearing loss in the general population.
Humans can hear sounds in the frequency range between about 20 Hz to 20,000 Hz. Difficulties hearing above 2000 Hz (2000 to 8000 Hz) is referred to as high frequency hearing loss. (To see if you can hear 2000 Hz sounds click here). About 1 in 7 people over 65 have sensorineural hearing loss. 90 % of people with hearing loss have the sensorineural hearing loss type.
What’s it like to have high frequency hearing loss?
Affected individuals may have trouble discriminating certain voices (children and female), birds, animal sounds, beeps from phones and appliances, and sometimes door bells. Individuals with high frequency hearing loss may find it difficult to have conversations when there is a lot of background noise present. They have difficulty with certain letters including “S, H and F …and TH” Affected people have trouble conversing in restaurants and at parties. Some patients also have tinnitus, which is often seen in those with sensorineural hearing loss.
Hearing aids can help high frequency hearing loss and are specifically designed for specific patterns of hearing loss.
REFERENCE
Kuang-Hsu Lien, TzoTzong-Yun Ger, Ching-Chi Chi. Association of alopecia areata with sensorineural hearing loss: a systematic review and meta-analysis. Dermatology. 2023 Apr 24.
Patients with Periodontitis May Be at Increaed risk for Alopecia Areata
Periodontitis and Gingivitis
Periodontitis is a gum disease. It starts with inflammation of the gingiva (gingivitis) but then spreads deeper. This inflammation can then spread to below the gums and along the roots of the teeth. The result is permanent damage to the tissues (or “periodontal ligament”) around the teeth and to the supporting bone. Teeth start to loosen and can eventually be lost.
Therefore, patients with gingivitis can develop periodontitis if they don’t treat their gingivitis. Periodontitis is a much more serious form of gum disease. About 50 % of the population has gingivitis and peridontitis itself is less common.
Gingivitis is an inflammation that is limited to the gum line, while periodontitis is associated with loss of the jawbone, periodontal ligament, and root cementum.
Patients may not notice any signs or symptoms whatsoever but may notice swollen and puffy gums, increased bleeding from the gums when they eat or brush their teeth, bad breath, receding gums giving the appearance of longer teeth and painful chewing.
Periodontitis is markedly influenced by oral hygiene and good brushing of the teeth. However, other risk factors are relevant including smoking, genetics, age, diet, type 2 diabetes, stress:
Recent evidence indicates that periodontitis is a type of autoimmune disease. In fact, several studies have demonstrated the involvement of autoimmune responses in this condition. Bacteria in the dental plaque induce antibody formation. Autoreactive T cells, natural killer cells, autoantibodies, and genetic factors are reported to have an important role in the autoimmune component of periodontal disease
In addition, periodontitis is associated with immune-mediated cutaneous and systemic inflammatory disorders, such as psoriasis, systemic lupus erythematosus and rheumatoid arthritis
Kim et al 2022
There have been sporadic reports in the literature of associations between dental disease and alopecia areata.
Authors from Korea set out to investigate whether periodontitis increases the risk of AA by using the National Health Insurance Service claims database. They compared 68,000 patients with periodontitis that were matched to 68,000 patients without periodontitis.
There was statistically significant higher AA development in the periodontitis group (a-HR: 1.36 (95% confidence interval [CI]: 1.28–1.44); This was true for all the clinical subtypes of AA including patchy AA, 1.39 [CI: 1.31–1.49]; alopecia totalis/universalis, 1.49 [CI: 1.20–1.85].
Children and Young Adults with Periodontitis at Higher Risk for AA
In further subgroup analysis of the data, children and young adults had a significantly higher risk of AA than older adults (a-HR 2.01 [CI: 1.79–2.25] and 2.06 [CI: 1.92–2.21], respectively).
Patients with Periodontitis Are At Risk Not Only for AA but other Autoimmune Diseases
Authors also showed that the periodontitis group had a significantly higher risk of other autoimmune diseases (known to be AA comorbidities) including systemic lupus erythematosus (a-HR, 2.97 [CI: 1.54–5.74]), rheumatoid arthritis (a-HR, 1.18 [CI: 1.02–1.36]), and atopic dermatitis (a-HR, 1.22 [CI: 1.08–1.38]).
Conclusion
The study showed an association between periodontitis and alopecia areata. Patients with peridontitis may be at risk to develop alopecia areata. The mechanism by which periodontitis increases the risk of AA is not known and was not the focus of this study. It has been proposed that there is a common underlying autoimmune -inflammatory nature of both conditions and patients with periodonitis had a greater chance of many autoimmune disease.
Although the exact mechanism by which periodontitis acts as a risk factor for AA has not yet been identified, it could be explained by the common autoimmune-inflammatory nature of the two disorders.
REFERENCE
Kim JS et al. Periodontitis and risk of alopecia areata: A nationwide population-based cohort study in Korea. J Eur Acad Dermatol Venereol. 2022 Nov 17.
Retinopathy, Retinal Vascular Occlusion and Retinal Detachment Increased in Alopecia Areata
A number of prior studies have questioned whether patients with alopecia areata have eye abnormalities. For example, a 2014 study suggested that up to 7 % of patients with alopecia areata had retinal degeneration.
A new study from Taiwan set out to examine the relationship between alopecia areata and retinal diseases. By examining information found in the National Health Insurance Research Database in Taiwan, the authors compared 9909 patients with alopecia areata to 99,090 matched controls.
Compared with the control patients, patients with alopecia have an approximately 3 fold greater risk of having a retinal disease ( adjusted hazard ratio (aHR) of 3.10 (95% confidence interval [CI] 2.26-4.26). Of the various retinal diseases studied, patients with alopecia areata had significantly higher risks of developing retinal detachment (aHR 3.98; 95% CI 2.00-7.95), retinal vascular occlusion (aHR 2.45; 95% CI 1.22-4.92), and retinopathy (aHR 3.24; 95% CI 2.19-4.81) than controls.
Conclusions
The conclusion of this study was that patients with alopecia areata had a significantly higher risk of retinal diseases compared to controls. More studies are needed to confirm these findings and determine why these connections might exist.
REFERENCE
Ting H-C et al. Association between alopecia areata and retinal diseases: A nationwide population-based cohort study. J Am Acad Dermatol . 2021 Nov 1;S0190-9622(21)02735-3.
Alterations in Corneal Sensitivity, Staining and Biomechanics of Alopecia Areata Patients
A recent study examined corneal sensitivity, staining, and biomechanics in patients with severe alopecia areata. This was published in the Journal of Clinical Medicine in 2024.
Alopecia areata, an autoimmune disorder known for causing hair loss, has shown associations with various eye-related health issues. However, the relationship between alopecia areata and specific corneal changes has not been thoroughly investigated until now.
Burgos-Blasco B et al. 2024
The researchers conducted a case-control study to investigate the connection between alopecia areata and certain changes in the cornea. They enrolled 25 patients suffering from severe alopecia areata, defined as having over 50% scalp involvement according to the Severity of Alopecia Tool. These patients were compared to 29 control participants who did not have the condition. All participants were adults over 18 years old and had not undergone any recent systemic treatment for alopecia areata.
The study involved a comprehensive series of ophthalmological evaluations. These evaluations included assessing visual acuity, measuring corneal sensitivity using the Cochet–Bonnet esthesiometer, and conducting slit-lamp biomicroscopy. Furthermore, corneal topography was analyzed with Pentacam, and corneal biomechanics were examined using Corvis scheimpflug technology. The study focused on various outcomes, including visual acuity, refractive error, corneal aerometry, and biomechanical factors such as applanation lengths, velocities, and the Corvis Biomechanical Index, along with topographic measurements.
What were the results?
Patients suffering from alopecia areata demonstrated a significant decrease in corneal sensitivity compared to the control group, with a p-value of less than 0.001. Additionally, these patients experienced increased corneal staining (p = 0.004), which was notably associated with more advanced cataracts, also showing a p-value below 0.001.
When examining corneal topography, measurements such as the anterior topographic flat meridian, average anterior keratometry, and the maximum keratometric point were all found to be higher in the alopecia areata group (p ≤ 0.040).
In contrast, the pachymetry readings indicated thinner corneas in these patients (p ≤ 0.001). From a biomechanical standpoint, significant alterations were observed as well. Patients with alopecia areata had shorter applanation lengths (p ≤ 0.029) and a higher Corvis Biomechanical Index (p = 0.022). Worryingly, within this group, two individuals were diagnosed with keratoconus, and four other eyes exhibited signs of subclinical keratoconus.
Conclusions
This research highlights notable changes in corneal sensitivity, increased staining, and significant shifts in corneal biomechanics and topography in patients with severe alopecia areata. These results indicate that those with alopecia areata might have a higher risk of developing keratoconus. It’s important to consider whether eye doctors should be performing more regular checks for eye-related issues in these patients.
To summarize, this emphasizes the need for consider detailed eye exams in patients with alopecia areata, particularly in severe cases. Spotting potential eye problems like keratoconus early on can lead to timely treatments and improved outcomes for patients.
REFERENCE
Burgos-Blasco B et al. Alterations in Corneal Sensitivity, Staining and Biomechanics of Alopecia Areata Patients: Novel Findings in a Case-Control Study. J Clin Med . 2024 Apr 21;13(8):2426. doi: 10.3390/jcm13082426.
Five Fold Higher Risk of Developing Alopecia Areata Among Individuals with PTSD
Five Fold Higher Risk of Developing Alopecia Areata Among Individuals with PTSD
It is clear that stress can impact the immune system and the subsequent risk of developing various autoimmune disease. An increasing number of research studies are examining how posttraumatic stress disorder impacts the development of various autoimmune diseases.
Posttraumatic stress disorder (PTSD) is a psychiatric disorder that may occur in people who have experienced or witnessed a traumatic event or series of events or set of circumstances. It has been estimated that PTSD affects up to 1 in 11 people during their entire lifetime. Every year PTSD affects about 3.5 % of the US population.
Dai et al 2021: A New Study Linking PTSD with increased Risk of AA
A new study by Dai et al aimed to investigate the association of PTSD with the risk of autoimmune skin diseases in Taiwan.
Participants were recruited from the National Health Insurance Research Database in Taiwan. The authors included approximately 9,800 patients with PTSD and 39,000 matched controls. After adjusting for confounders, the authors found a threefold increased risk of autoimmune skin diseases among the patients with PTSD (adjusted hazard ratio [aHR] = 3.00, 95% confidence interval [CI] = 2.21-4.07) compared with that among matched controls.
When the authors examined specific skin diseases, there were statistically significant associations found between PTSD and lichen planus (aHR = 31.63, 95% CI = 4.00-249.91), vitiligo (aHR = 16.06, 95% CI = 4.48-57.54), autoimmune bullous diseases (aHR = 9.55, 95% CI = 1.98-45.99), alopecia areata (aHR = 4.77, 95% CI = 2.47-9.20), and psoriasis (aHR = 3.81, 95% CI = 1.90-7.67).
.dpuf
Conclusion
All in all, this study supported the notion that that patients with PTSD had an increased risk of developing a variety of autoimmune skin diseases compared with the matched controls.
REFERENCE
Dai Y-X et al. Posttraumatic Stress Disorder and the Associated Risk of Autoimmune Skin Diseases: A Nationwide Population-Based Cohort Study. Psychosom Med. 2021 Apr 1;83(3):212-217. doi: 10.1097/PSY.0000000000000920.
What diseases are increased and decreased among patients with alopecia areata?
What diseases are increased and decreased among patients with alopecia areata?
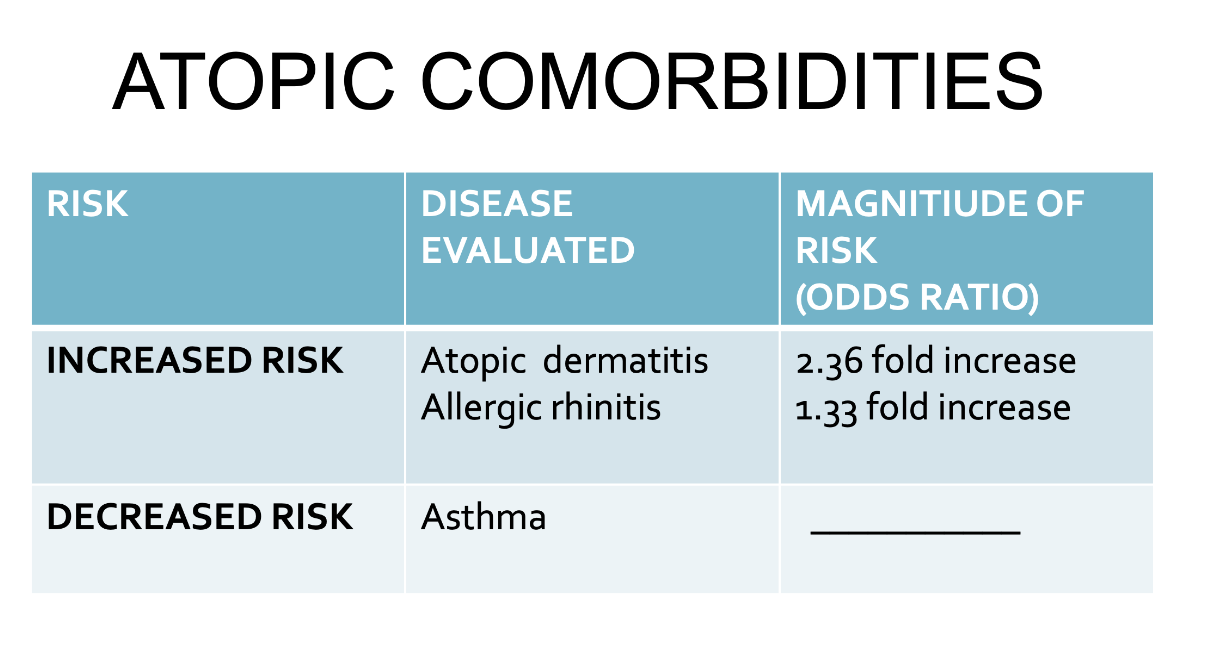
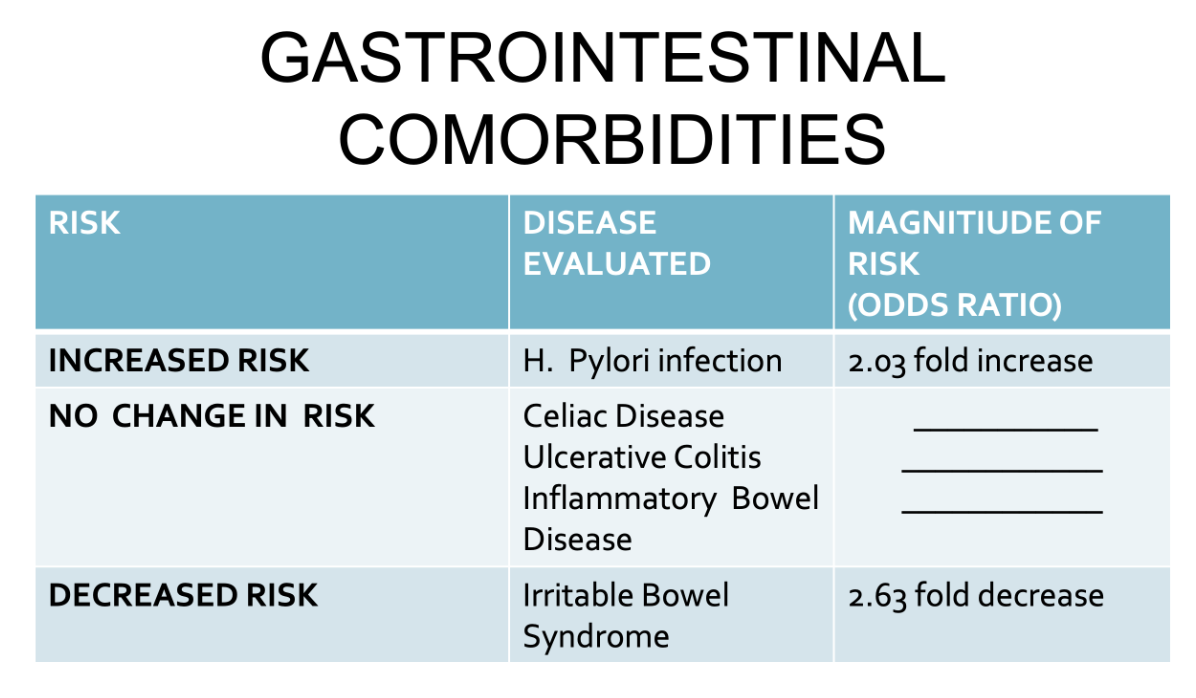
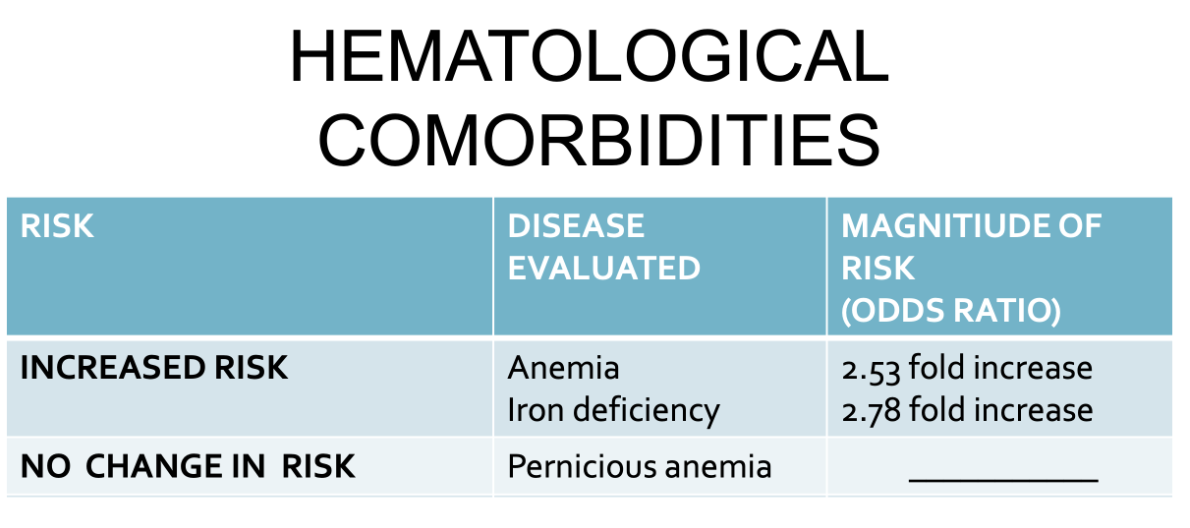
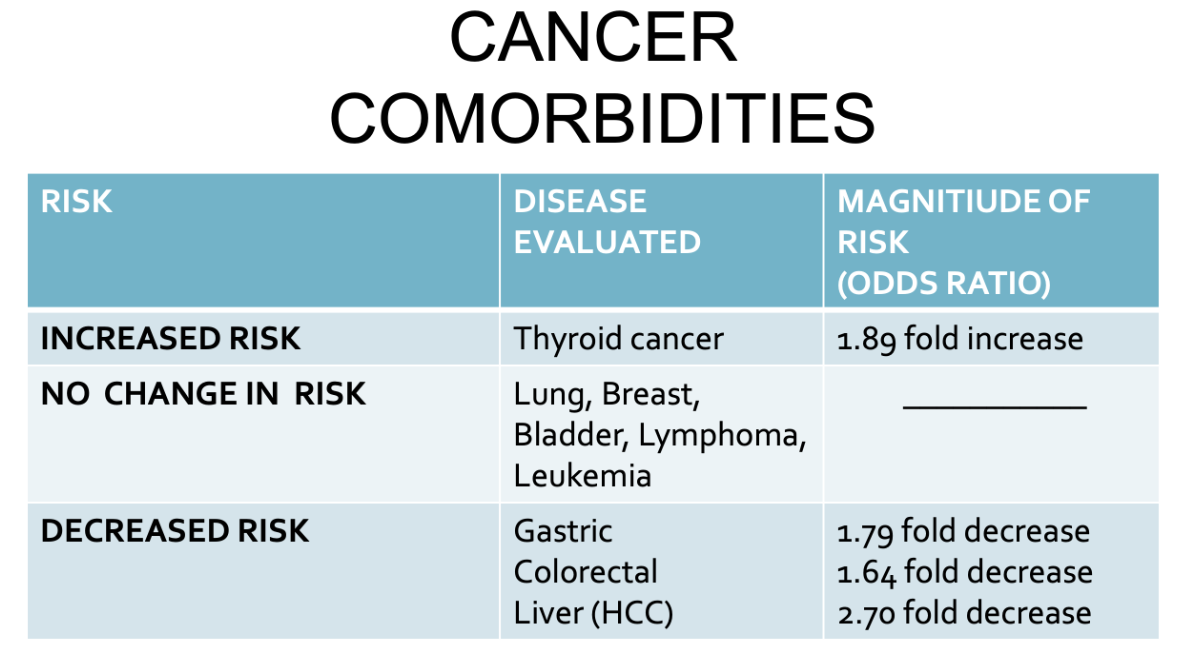
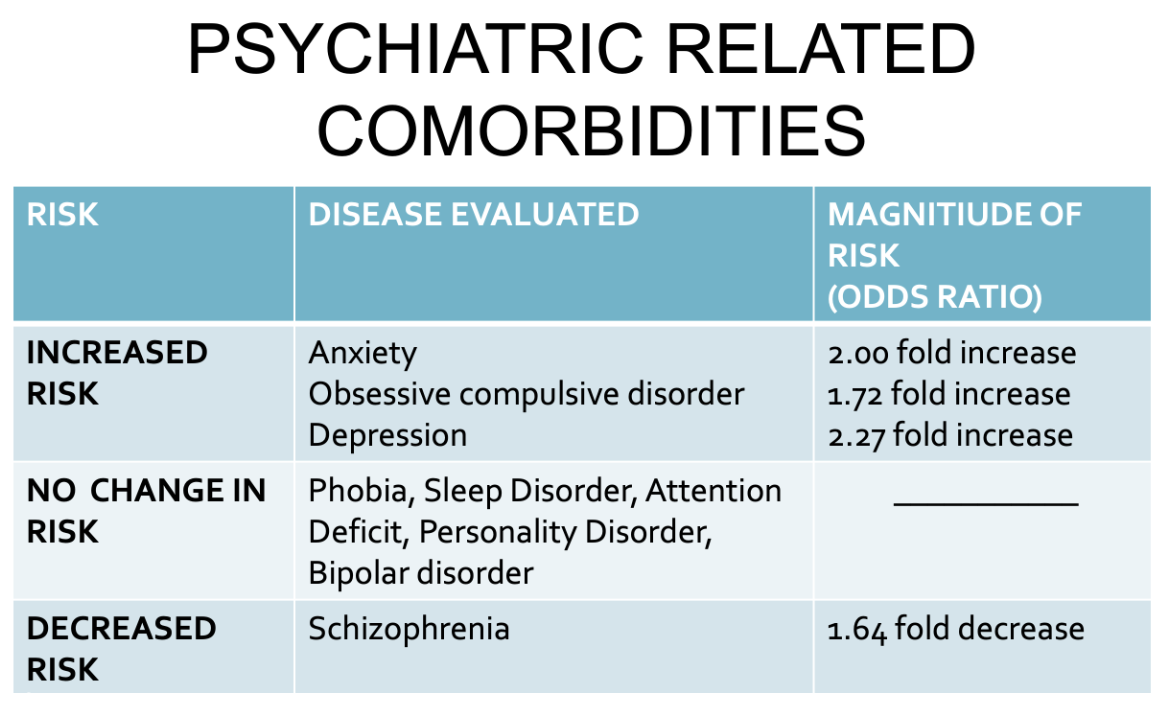
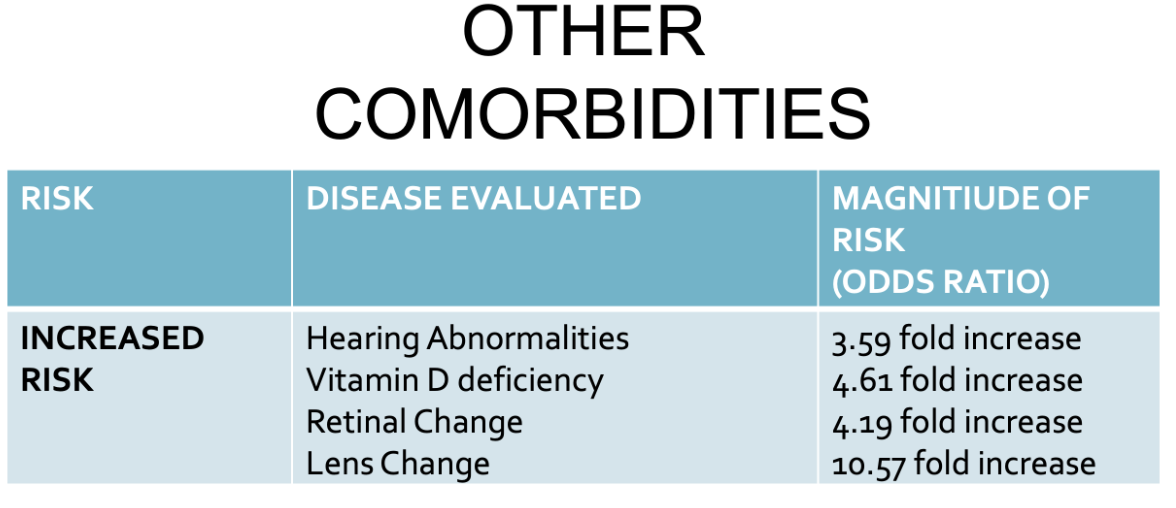
A 2019 meta-analysis sought to determine the health conditions that are increased or decreased in patients with alopecia areata. Lee and colleagues from South Korea evaluated 87 published studies.
I have highlighted here some of the very interesting findings of the study.
Conclusion and Summary
This is a wonderfully helpful meta-analysis which summarizes some of the key associations in alopecia areata. Alopecia is associated with an increased risk of atopic dermatitis, hyperinsulinemia, metabolic syndrome, lupus, H. pylori infection, vitamin D and iron deficiency, thyroid dysfunction, thyroid cancer, anxiety , depression and obsessive compulsive disorder.
Reference
Lee S et al. Comorbidities in alopecia areata: A systematic review and meta-analysis. .J Am Acad Dermatol. 2019 Feb;80(2):466-477.e16.
Altered Immune System Function Leads to Increased Risk of Alopecia Areata in Down Syndrome
It’s well known that patients with Trisomy 21 (Down syndrome) are at increased risk for a variety of immune mediated and autoimmune mediated medical conditions.
Dermatological Conditions that may be more common in Down Syndrome include:
Dry Skin and Ichthyosis
Keratosis pilaris
Pityriasis rubra pilaris
Elastosis perforans serpiginosa
Seborrheic Dermatitis
Palmoplantar keratoderma
Psoriasis
Cafe au lait macules
Lumbosacacral dermal melanosis
Syringomas
Geographic tongue
Angular cheilitis
Vitiligo
Alopecia areata
Fungal infections
Folliculitis
Lichen nitidus
Hidradenitis
Blood disorders
Alopecia Areata In Patients with Trisomy 21
I read with interest a recent study that examined the prevalence of different immune related diagnoses in a cohort of 1299 patients with Down syndrome compared to a 2605 patient control cohort at the Mount Sinai Health System in New York, NY. The evaluation spanned about 18 years of data. Individuals with trisomy 21 had a six fold higher odds of alopecia areata compared to controls (OR 6.06, p = 0.01).
Other conditions that were increased in alopecia areata included sepsis (OR 4.79, p < 0.001), purpura and other hemorrhagic conditions (OR 2.31, p < 0.001), rosacea (OR 3.11, p < 0.001). In this particular study, there was a lower odds of a diagnosis of herpesviral infection (OR 0.42, p = 0.01), and viral warts (OR 0.51, p = 0.04).
Comment and Summary
It’s well known that the immune system functions slightly differently in patients with Trisomy 21 compared to controls. Past studies have highlighted several skin issues that are more common in patients with Trisomy 21. Alopecia areata is more common in patients with Trisomy 21 and past studies have put the number at around 10 % (compared to 2 % in the general population). This study by Gansa et al agrees with the general trend of prior data. Alopecia areata in patients with Down Syndrome tends to give more hair loss than seen in patients without Down syndrome.
REFERENCE
Gansa W et al. Dysregulation of the Immune System in a Natural History Study of 1299 Individuals with Down Syndrome. J Clin Immunol. 2024 May 22;44(6):130. doi: 10.1007/s10875-024-01725-6.
Women with PCOS May be More likely to have Children with ADHD
Polycystic ovarian syndrome (PCOS) is a hormonal disorder in women. It is not one condition but a constellation of symptoms. Patients with PCOS typically have evidence of hyperandrogenism (excess male-type hormones) and irregular periods. Women with PCOS typically have cysts present in the ovaries but some do not. The exact cause of PCOS remains unknown although a genetic component is likely for many women. The ovaries of women with PCOS are known to secrete higher levels of male hormones which contributes to irregular periods and infertility. Women with PCOS may seek medical attention for a variety of reasons including insulin resistance, diabetes, high blood pressure, acne, increased hair growth on the face, irregular periods, infertility. Women with PCOS may also present to a hair clinic with concerns about androgenetic alopecia. It is therefore extremely important that hair specialists understand this condition.
New Research on Children born to Mothers with PCOS
A great deal of research is currently being conducted into the cause of PCOS and how it affects women. Research is also being conducted into the health of babies born to mothers with PCOS. Research has suggested that the hormonal changes in utero influence the development of the fetus.
One issue that has been studied is the risk of attention-deficit/hyperactivity disorder (ADHD) in babies born to mothers with PCOS. ADHD is the most common childhood neurodevelopment disorder. Male hormones may play a role as boys are two to three times more likely to develop ADHD.
A study by Berni and colleagues of over 16,000 women showed that women with PCOS have a slight risk of giving birth to children with attention deficit hyperactivity disorder (ADHD) and Asperger syndrome.
Kosidou and colleagues performed a matched case-control study using health and population data registers for all children born in Sweden from 1984 to 2008. In their study, a total of 58,912 ADHD cases (68.8% male) were identified and matched to 499,998 unaffected controls by sex and birth month and year. The results indicated that Maternal PCOS increased the odds of offspring ADHD by 42% after adjustment for confounders (odds ratio [OR], 1.42; 95% confidence interval [CI], 1.26-1.58). The risk for ADHD was even higher among obese mothers with PCOS and was highest among obese mothers with PCOS and other features of metabolic syndrome.
Conclusion
Recent research suggests that differences in maternal hormones during pregnancy in women with PCOS affect the chances of having children with ADHD and possible other neurodevelopmental issues. Overall the risk is low.
REFERENCES
Berni TR, et al. Polycystic ovary syndrome is associated with adverse mental health and neurodevelopmental outcomes. J Clin Endocrinol Metab. 2018.
Kosidou K, et al. Maternal Polycystic Ovary Syndrome and Risk for Attention-Deficit/Hyperactivity Disorder in the Offspring. Biol Psychiatry. 2017.
Alopecia Areata and the Risk of Thyroid Cancer
It’s well known that patients with alopecia areata are at increased risk for thyroid abnormalities. In fact, autoimmune thyroid disease is among the most common comorbidities seen with alopecia areata. One association which seems real - but quite unexpected - is the increased risk of thyroid cancer that patients with alopecia areata might have.
In 2018, Lee et al performed a study to better understand the cancer risks in patients with alopecia areata. The authors studied 668,604 patients who were treated for alopecia from 2007 to 2014 and compared data to age- and sex-matched control subjects. Compared to controls, AA patients had a 4 % increase in overall cancer risks (hazard ratio (HR), 1.043; 95% confidence interval (CI), 1.022-1.065 and patients with AT/AU had a 7% increased risk ( HR, 1.07; 95% CI, 1.013-1.129, respectively).
The authors found that the risks of cancers of the oral cavity, esophagus, liver, biliary tract, pancreas, larynx, lung, kidney, breast, cervix, ovary, uterus, testis, nerve, skin cancers; and lymphoma, multiple myeloma, and leukemia, were not increased in alopecia patients. An increased risk of thyroid cancer was identified in patient with AA or AT/AU. In AA patients alone, the risks of bladder and prostate cancers were increased.
Other studies linking thyroid cancer and alopecia areata
A 2019 meta-analysis by Lee and colleagues sought to determine the health conditions that are increased or decreased in patients with alopecia areata. The authors evaluated 87 published studies. Regarding cancer risk in patients with alopecia areata, they identified a nearly two fold increased risk of thyroid cancer. There was no increased risk for lung, breast, bladder, lymphoma and leukemia. The authors identified decreased risk of gastric, colon and liver cancer.
In 2021, Lugović-Mihić described a patient with AA of the beard and thyroid cancer.
Final Comment
There is enough data accumulating now to convincingly show that patients with alopecia have a higher risk of cancer. The magnitude of risk overall is fairly small. The risks appear small enough that screening guidelines have not been introduced. Everyone with alopecia areata requires a TSH. However, it’s important to be aware that TSH levels are usually normal in patients with thyroid cancer. Patients with a lump in the neck, difficulty swallowing, a pain in the neck, swelling in the neck, a feeling that shirt collars are too tight, a change in the voice (to a hoarse voice) or patients with enlarged lymph nodes in the neck require further evaluation for possible thyroid cancer.
The findings of these studies are important. Patients with alopecia totalis and universalis are probably at even greater risk than patients with less severe forms (like patchy AA). This is backed up by a 2023 study by George et al.
There is something special about thyroid cancer. It stands out as a type of cancer that is clearly increased in patients with AA. It may not be the only cancer that is increased as patients with alopecia totalis and universalis have a higher rate of non-melanoma skin cancer, melanoma skin cancer, and lymphoma compared to patients with milder forms and compared to the general population.
REFERENCES
Lee JH et al. Cancer risk by the subtype of alopecia. Sci Rep . 2018 Jun 27;8(1):9748. doi: 10.1038/s41598-018-28142-1.
Lee S et al. Comorbidities in alopecia areata: A systematic review and meta-analysis. J Am Acad Dermatol. 2019 Feb;80(2):466-477.e16.
Lugović-Mihić L et al. CAN SKIN BE A MARKER FOR INTERNAL MALIGNANCY? EVIDENCE FROM CLINICAL CASES. Acta Clin Croat . 2021 Dec;60(4):711-721. doi: 10.20471/acc.2021.60.04.19.
George P et al. Incidence Rates of Infections, Malignancies, Thromboembolism, and Cardiovascular Events in an Alopecia Areata Cohort from a US Claims Database., Dermatol Ther (Heidelb). 2023 Aug; 13(8): 1733–1746.
PCOS and the Risk of Alopecia Areata
Patients with PCOS May Have a Three Fold increased Risk for Alopecia Areata
Polycystic ovary syndrome (PCOS) is a common endocrine condition in women. In fact, up to 10-15 % of women of child-bearing age have PCOS. Women present with irregular periods, infertility, acne, hirsutism and sometimes androgentic alopecia.
There is emerging evidence that women with PCOS are at risk for some autoimmune diseases. In fact, a 2018 meta-analysis that we reviewed in the past suggested that women with PCOS have a 2 to 4 fold increased risk of autoimmune thyroid disease.
Whether women with PCOS are at increased risk for the autoimmune mediated hair loss condition alopecia areata has only recently started to be carefully explored.
In 2017, Ranasinghe and colleagues showed women with PCOS frequently had androgen excess and many women with androgen excess had a diagnosis of PCOS. In fact, the researchers noted that androgen excess/PCOS was the most common dysfunction identified in 220 patients with AA and all subtypes 42.5% (n=96) (p<0.001). It should be noted that the 2017 Ranasinghe study was not designed to evaluate the magnitude of increased risk for androgen excess or PCOS in patients with alopecia areata.
Overall, the researchers noted that androgen excess/PCOS was the most common dysfunction identified in 220 patients with AA and all subtypes 42.5% (n=96) (p<0.001).
Is the Risk of Alopecia Areata Increased in PCOS?
Researchers from Taiwan set out to evaluate whether patients with PCOS are at increased risk of having a diagnosis of alopecia areata. Their retrospective cohort study compared 10 967 patients with PCOS to 43 868 matched controls. Individuals with PCOS were found to have a 3 fold increased risk of having a diagnosis of alopecia areata (adjusted HR, 3.12; 95% CI, 1.81–5.40; P < 0.001).
Conclusion
This is an interesting study which complements the growing body of literature suggesting that a proportion of women with alopecia areata may have androgen excess and PCOS. This particular study gives us a number - suggesting that women with PCOS have a three fold increased risk of having a diagnosis of alopecia areata.
This study is important as it draws attention to these potential links. Female patients with alopecia areata need to be asked about acne, irregular periods, hirsutism, infertility just like all women with hair loss do! Women with alopecia areata age 16-45 who have regular periods and do not have acne, hirsutism or known infertility do not generally need extensive work ups. However women with alopecia areata age 16-45 who do not have regular menstrual cycles or have acne, hirsutism or infertility should have appropriate screening to rule out androgen excess and PCOS.
REFERENCE
Chang et al. Increased risk of alopecia areata among patients with polycystic ovary syndrome: A population-based cohort study. J Dermatol. 2021 Feb;48(2):242-244.
Romitti et al. Association between PCOS and autoimmune thyroid disease: a systematic review and meta-analysis. Endocr Connect. 2018 Oct 26;7(11):1158-1167.
Ranasinghe GC, Piliang M, Bergfeld W (2017) Androgen Excess in Alopecia Areata, an Unexpected Finding. Med J Obstet Gynecol 5(3): 1104.
Male Balding and Kidney Stones: Is there a risk?
Authors of a 2016 study set out to determine if patients with male balding (male androgenetic alopecia) had an increased risk of urolithiasis (kidney stone disease).
There were 302 male patients in the study and patients were classified according to the degree of baldness. Patients with no baldness were classified as Group I. Patients with AGA in the frontal region (Hamilton Norwood stages II, III, IIIa, and IVa) were classified as Group II. Those with hair loss in the vertex region (HNS stage III-vertex, V) were classified as Group III. Finally, patients with hair loss in both vertex and frontal regions (HNS stages IV, Va, VI, and VII) were classed as Group IV.
The presence of urinary tract stones was detected in 28.9% of patients in Group I; 26.5% of Group II; 36.9% of Group III; and 44.4% of Group IV (p = 0.085). In patients aged under 60, urinary stone disease was statistically significantly associated with advanced balding. Stones were detected in 30.8% of patients in Group I; 26.4% of Group II; 41.2% of Group III; and 53.8% of Group IV (p = 0.001). In patients aged over 60, the data was not significant. Urolithiasis was detected in 12.5% of patients in Group I; 26.9% of Group II; 32.2% of Group III; and 37.8% of Group IV (p = 0.371).
Conclusions and Comments
This is one of the first studies to suggest a correlation between vertex pattern hair loss in males and kidney stones in patients - especially in those under age 60. The reasons for this increased risk are not entirely clear, but it is understood that testosterone may influence stone formation in some males. Other factors may be relevant but were not studied in this particular study
REFERENCE
Resorlu M et al. The association of urolithiasis and androgenetic alopecia. Ren Fail. 2016;38(1):84-8. doi: 10.3109/0886022X.2015.1096729. Epub 2015 Oct 13.
Are patients with PCOS at Increased Risk for Ovarian, Endometrial or Cervical Cancer?
Past studies have suggested that women with polycystic ovary syndrome (PCOS) are at increased risk for endometrial cancer (uterine cancer). Whether or not patients with PCOS are at increased risk for other gynecological cancers - such as ovarian or cervical cancer is not clear. Past studies have presented mixed results.
Abu-Zaid A et al. 2024
Authors of a new study set out to systematically examine the relationship between polycystic ovary syndrome and ovarian, endometrial, and cervical cancers using the National Inpatient Sample (NIS) database. The NIS database is the largest publicly available all-payer inpatient care database in the United States.
Authors assessed the database between the years 2016 to 2019 to evaluate association between PCOS and gynecologic cancers. Overall, 15,024,965 patients were analyzed, of whom 56,183 patients were diagnosed with PCOS and 14,968,782 patients did not have PCOS. Among the 91,599 patients diagnosed with gynecologic cancers, there were 286 with PCOS and 91,313 without PCOS.
Multivariate analysis showed that PCOS was significantly associated with a higher risk of endometrial cancer (OR = 3.90, 95 % CI [4.32-4.59], p < 0.0001). There was no significant correlation between PCOS and risk of ovarian cancer (OR = 1.09, 95 % CI [0.89-1.34], p = 0.409) and cervical cancer (OR = 0.83, 95 % CI [0.62-1.11], p = 0.218).
Comments
This is an interesting study and follows the general view that PCOS is associated with an increased risk of uterine (endometrial) cancer but not an increased risk of ovarian or cervical cancer.
Treatments such as birth control pills may reduce the risk of endometrial cancer, although this was not specifically addressed in this study.
REFERENCE
Abu-Zaid A et al. Association between polycystic ovary syndrome and the risk of malignant gynecologic cancers (ovarian, endometrial, and cervical): A population-based study from the U.S.A. National Inpatient Sample 2016-2019. Eur J Obstet Gynecol Reprod Biol. 2024 Jun 23:299:283-288. doi: 10.1016/j.ejogrb.2024.06.031. Online ahead of print.
Bidirectional Relationship Between AA and Psoriasis
There is something very unique about the relationship between alopecia areata and psoriasis. We know that many patients we see with alopecia areata have psoriasis and many patients with psoriasis have alopecia areata.
Jung JM et al. 2022
In 2022, authors from South Korea set out to examine the relationship between psoriasis and alopecia areata. The reviewed published studies in the medical literature in order to answer the questions:
Are patients with alopecia areata more likely to develop psoriasis?
Are patients with psoriasis more likely to develop alopecia areata?
The authors included 27 studies in their meta-analysis. The authors calculated that the pooled odds ratio of alopecia areata among patients with psoriasis was 2.71 (95% CI, 2.29-3.21), and the pooled odds ratio of psoriasis among patients with alopecia areata was 3.52 (95% CI, 1.27-9.74).
Comments
Alopecia areata psoriasis have a unique bidirectional relationship. Patients with psoriasis are at increased risk for AA and patients with AA are at increased risk for psoriasis.
REFERENCE
Jung JM et al. Association between psoriasis and alopecia areata: A systematic review and meta-analysis. J Dermatol. 2022 Sep;49(9):912-915. doi: 10.1111/1346-8138.16420. Epub 2022 May 5.
CCCA and Uterine Fibroids
There is a Five Fold increased Risk of Fibroids in Women with CCCA
A study, published in JAMA Dermatology, has given evidence that women with central centrifugal cicatricial alopecia (CCCA) are at increased risk of developing benign uterine tumors known as fibroids. The medical term for fibroids is uterine leiomyomas.
CCCA is a type of scarring alopecia that occurs predominantly in women with afro-textured hairs. This new data suggests that a genetic predisposition to develop excessive scar tissue in other area of the body may be central to the underlying mechanisms that cause these two diseases.
The researchers analyzed data from over 487,000 black women and examined the incidence of fibroids in women with CCCA and those without CCCA. Out of 486,000 women in the general population, 3.3 % had fibroids. However, 13.9 % of women with CCCA were found to have fibroids. Taken together, this works out to a five-fold increased risk of fibroids in women with CCCA.
Conclusion
There appears to be an increased risk of uterine fibroids in women with CCCA. Whether there is an increased risk of other scarring-related diseases of the body warrants further study.
REFERENCE
Dina et al. Association of Uterine Leiomyomas With Central Centrifugal Cicatricial Alopecia. JAMA Dermatology, 2017; DOI: 10.1001/jamadermatol.2017.5163
Patients with Alopecia Areata are At Increased Risk for Joint Disease
In 2023, Kincaid et al performed a case-control study to examine whether patients with alopecia areata were at increased risk for arthritis.
About 46,000 cases and 46,000 controls were compared. Data showed that patients with AA had a significantly higher risk (compared to controls) of developing:
psoriatic arthritis (OR = 2.344, P < .0001)
rheumatoid arthritis (OR = 2.09, P < .0001)
ankylosing spondylitis (OR = 1.68, P = .0021)
The mean age of these AA-arthritis subgroup cohorts at the time of data collection was 49.2, 52.1, and 44.3 years old, respectively. Patients with both AA and inflammatory arthritis were mainly female, with a large proportion being in the AA and rheumatoid arthritis subgroup.
Interestingly, alopecia areata was also found to be associated with the development of “other crystal arthropathies” (OR, 1.763; P < .0001; mean age, 67.3 years old) and “other inflammatory arthropathies” (OR, 1.631; P < .0001; mean age, 56.2 years old). However, the joint disease gout occurred at similar rates between the cohorts.
REFERENCE
Colin M Kincaid, Ajay N Sharma, Natasha A Mesinkovska. Alopecia areata is associated with risk of inflammatory arthritis. J Am Acad Dermatol. 2023 Aug;89(2):422-423. doi: 10.1016/j.jaad.2023.04.039. Epub 2023 Apr 28.
ALOPECIA AREATA AND ITS ASSOCIATION WITH POLLEN, DUST, AND CAT ALLERGIES
Authors from China recently performed a large study to assess the relationship between alopecia areata and various allergic conditions, including hay fever, eczema, asthma, and pollen, dust, and cat allergies.
Interestingly, the authors’ data showed a significant genetic correlation between atopy/allergies and an increased risk of developing alopecia. Notably, strong associations were observed for eczema, hay fever, asthma, and specific pollen, dust, and cat allergies. All these conditions are associated with an increased risk of developing alopecia areata.
The authors conclude that there is compelling genetic evidence of an association between atopic and allergic conditions and the development of alopecia areata.
Does blocking allergies help alopecia areata? A Closer Look at Two Studies!
It’s increasingly clear that blocking allergic responses can be part of an effective treatment strategy for alopecia areata.
Zeng et al., 2023
In 2023, researchers set out to study if allergen immunotherapy (AIT) against house dust mite (HDM) allergy affects disease severity and prognosis for patients with alopecia areata. 69 patients with alopecia areata were studied. All had dust mite allergy. 34 patients received conventional/traditional AA treatment plus allergen immunotherapy against dust mites (group 1) and 35 patients received conventional/traditional AA treatment (group 2) alone. At the end of the 3-year desensitization course, Group 1 (treated with allergen immunotherapy) presented with better hair density than Group 2 (conventional treatment) - especially for those patients with less severe forms to start with and pre-adolescent alopecia totalis/universalis patients (age ≤ 14). In patients with elevated total IgE levels before starting allergy immunotherapy, a decrease in total IgE was correlated to a reduced extent of alopecia following completion of the allergy immunotherapy.
Kwon et al., 2023
In 2023, an interesting report in the Journal of Dermatology regarding house dust mite allergies highlighted the importance of treating dust mite allergies in patients with severe AA. The case was that of a 38-year-old man with alopecia areata and atopic dermatitis who presented to clinic with severe symptoms of both diseases. Despite using oral methylprednisolone (8 mg/day) and cyclosporine (100 mg/day) for 3 months, he has lost over 90% of his hair and his atopic dermatitis was rated as severe.
Total serum immunoglobulin E (IgE) levels were 4454 kU/L (normal <100 kU/L) and the specific IgE levels for dust mites were high. Treatment began with subcutaneous allergen immunotherapy against dust mites along with oral cyclosporine (100 mg/day). Topical tacrolimus was also applied to eczematous areas on body. Antihistamines were used, as necessary, to reduce itching. Hair loss was almost completely improved 1 year after the start of allergen immunotherapy, and the skin lesions of atopic dermatitis also dramatically improved. All in all, this is another nice report of how a comprehensive treatment plan for alopecia areata must address environmental triggers where possible. This patient had great results with immunotherapy.
Conclusion and Comments
All in all, data continues to emerge that certain environmental triggers are of significance in the pathogenesis of alopecia areata. Reducing their triggers and addressing these triggers helps regrow hair to some extent in patients with alopecia areata.
Practitioners need to address these triggers as part of a comprehensive management plan.
Treating alopecia areata is never about using template “one size fits all” treatment plans. It’s about understanding the patient’s comorbidities and addressing these comorbidities where appropriate. It’s about understanding each patient’s goals, risk tolerance, fears … and more!
All in all, we must consider allergen immunotherapy in patients with alopecia areata who have severe allergies.
REFERENCES*
Xu W et al. Genetic links between atopy, allergy, and alopecia areata: insights from a Mendelian randomization study. Allergy Asthma Clin Immunol. 2024 Apr 27;20(1):32. doi: 10.1186/s13223-024-00892-w
Zeng Z et al. Affiliations expandAllergen desensitization reduces the severity of relapsed alopecia areata in dust-mite allergic patients. Exp Dermatol . 2023 Jul;32(7):1108-1119. doi: 10.1111/exd.14819. Epub 2023 Apr 28.
Kwon IJ et al. Allergen-specific immunotherapy improves alopecia totalis in a severe atopic dermatitis patient. J Dermatol. 2023 Oct;50(10):1353-1356. doi: 10.1111/1346-8138.16841. Epub 2023 May 29.
If you have any questions about our courses, webinars or the Evidence Based Hair Fellowship, please contact the academy for more information at info@donovanhairacademy.com
Subscribe to receive new blogs by email